Islet Transplant for Type 1 Diabetes
Islet cell transplantation places cells from an organ donor into the body of another person. It is used experimentally to treat type 1 diabetes
|
|
| Image Courtesy of UCSF Diabetes Education Online |
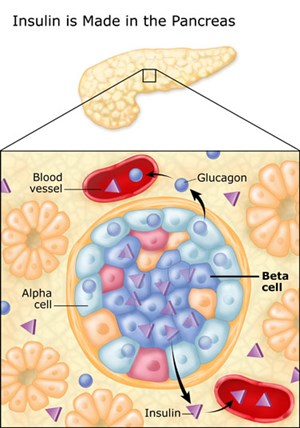
Pancreatic Islets and Beta Cells
The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas produce juices that help digest food and hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body to use and store energy from food.
Throughout the pancreas are clusters of cells called the islets of Langerhans. Islets are made up of several types of cells, including beta cells that make insulin. Insulin is a hormone that helps the body use glucose for energy.
Insulin and Diabetes
Diabetes develops when the body doesn't make enough insulin, cannot use insulin properly, or both, causing glucose to build up in the blood. Diabetes is a serious disease, which, if not controlled, can be life threatening. It is often associated with long-term complications that can affect every system and part of the body. Diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage.
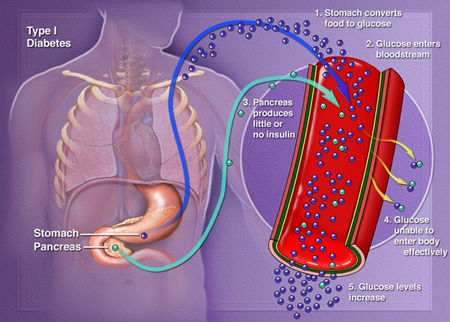
Type 1 Diabetes
Type 1 diabetes results from the body's failure to produce insulin, the hormone that "unlocks" the cells of the body, allowing glucose to enter and fuel them. It is an autoimmune disease in which the body views the beta cells (insulin producing cells found in the islets of the pancreas) as a foreign substance, so the patient's immune system attacks the islets and kills them. It is estimated that 5-10% of Americans who are diagnosed with diabetes have type 1 diabetes. Most people with type 1 diabetes do not have a family history of the disease and there is no way currently to prevent the onset of type1 diabetes.
 |
|
| Image courtesy of Clinical Islet Transplantation (CIT) Consortium, sponsored by National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK) and National Institute of Allergy and Infectious Diseases (NIAID) |
Insulin therapy, given by injection or insulin pump, is life-saving. However, it's not perfect. Most people with type 1 diabetes still have blood glucose levels that are above normal. This puts them at risk for the long-term complications of diabetes.
Some people have what doctors call labile, or brittle, diabetes. Blood glucose levels swing from high to low despite the best insulin plans.
Because of this, long-term type 1 diabetic survivors often develop vascular complications, such as diabetic retinopathy, an eye disease that can cause poor vision and blindness, and diabetic nephropathy, a kidney disease that can lead to kidney failure.
Hypoglycemia Unawareness
Those who are able to keep their blood glucose levels near normal often have trouble with low blood glucose (hypoglycemia). And after many years, some people lose the early symptoms that warn them that their blood glucose level is dropping. This is called hypoglycemia unawareness and raises the risk of severe hypoglycemia.
Hypoglycemia unawareness is a life-threatening condition that is not easily treatable with medication and is characterized by reduced or absent warning signals for hypoglycemia. Some Type 1 diabetic patients have been known to set their alarms to wake them several times a night out of fear they may have a catastrophic hypoglycemic episode while asleep. For such individuals, transplantation of pancreatic islets is a viable treatment option to consider.
Islet Cell Transplantation Procedure
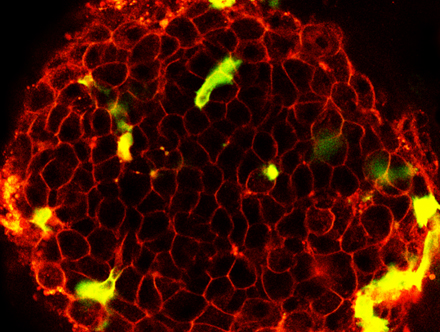
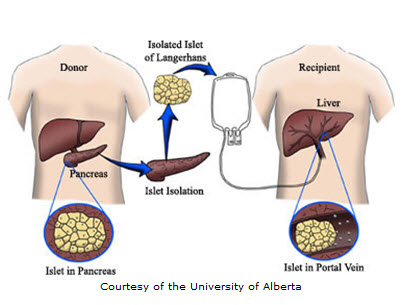
In islet transplantation, islets are taken from the pancreas of a deceased organ donor. The islets are purified, processed, and transferred into another person. Once implanted, the beta cells in these islets begin to make and release insulin. Researchers hope that islet transplantation will help people with type 1 diabetes live without daily injections of insulin.
Researchers use specialized enzymes to remove islets from the pancreas of a deceased donor. Because the islets are fragile, transplantation occurs soon after they are removed. Typically a patient receives at least 10,000 islet "equivalents" per kilogram of body weight, extracted from two donor pancreases. Patients often require two transplants to achieve insulin independence. Some transplants have used fewer islet equivalents taken from a single donated pancreas.
Transplants are often performed by a radiologist, who uses x rays and ultrasound to guide placement of a catheter-a small plastic tube-through the upper abdomen and into the portal vein of the liver. The islets are then infused slowly through the catheter into the liver. The patient receives a local anesthetic and a sedative. In some cases, a surgeon may perform the transplant through a small incision, using general anesthesia. Islets extracted from a donor pancreas are infused into the liver. Once implanted, the beta cells in the islets begin to make and release insulin.
 |
|
| Image courtesy of University of Alberta and the Clinical Islet Transplantation (CIT) Consortium, sponsored by National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK) and National Institute of Allergy and Infectious Diseases (NIAID) |
Islets begin to release insulin soon after transplantation. However, full islet function and new blood vessel growth associated with the islets take time. The doctor will order many tests to check blood glucose levels after the transplant, and insulin is usually given until the islets are fully functional.
Benefits and Risks Islet Transplantation
Benefits
The goal of islet transplantation is to infuse enough islets to control the blood glucose level without insulin injections. Other benefits may include improved glucose control and prevention of potentially dangerous episodes of hypoglycemia. Because good control of blood glucose can slow or prevent the progression of complications associated with diabetes, such as heart disease, kidney disease, and nerve or eye damage, a successful transplant may reduce the risk of these complications.
Risks
Risks of islet transplantation include the risks associated with the transplant procedure-particularly bleeding and blood clots-and side effects from the immunosuppressive drugs that transplant recipients must take to stop the immune system from rejecting the transplanted islets.
Most people need two infusions at different times to get enough islets that are working, and some need three. So, even if islet transplantation is found to be effective, currently, there are not enough donor pancreases available to treat everyone with type 1 diabetes.
Immunosuppression and Rejection
As with any organ transplant, the recipient of an islet transplant must take drugs every day to keep the body from rejecting the islets. The immune system is programmed to destroy bacteria, viruses, and tissue it recognizes as "foreign," including transplanted islets. In addition, the autoimmune response that destroyed transplant recipients' own islets in the first place can recur and attack the transplanted islets.
These drugs put the person at risk for infections and certain cancers. They can also cause side effects that range from mild to severe. Some people who received an islet transplant have had to stop taking these medications, because of side effects and then their new islets stopped working.
New Immunosuppression Protocols
The Edmonton protocol introduced the use of a new combination of immunosuppressive drugs, also called anti-rejection drugs, including daclizumab (Zenapax), sirolimus (Rapamune), and tacrolimus (Prograf). Daclizumab is given intravenously right after the transplant and then discontinued. Sirolimus and tacrolimus, the two main drugs that keep the immune system from destroying the transplanted islets, must be taken for life or for as long as the islets continue to function.
These drugs have significant side effects and their long-term effects are still not fully known. Immediate side effects of immunosuppressive drugs may include mouth sores and gastrointestinal problems, such as stomach upset and diarrhea. Patients may also have increased blood cholesterol levels, hypertension, anemia, fatigue, decreased white blood cell counts, decreased kidney function, and increased susceptibility to bacterial and viral infections. Taking immunosuppressive drugs also increases the risk of tumors and cancer.
Researchers continue to develop and study modifications to the Edmonton protocol drug regimen, including the use of new drugs and new combinations of drugs designed to help reduce destruction of transplanted islets and promote their successful implantation. These therapies may help transplant recipients achieve better function and durability of transplanted islets with fewer side effects. The ultimate goal is to achieve immune tolerance of the transplanted islets, where the patient's immune system no longer recognizes the islets as foreign. If achieved, immune tolerance would allow patients to maintain transplanted islets without long-term immunosuppression.
Researchers are also trying to find new approaches that will allow successful transplantation without the use of immunosuppressive drugs. For example, one study is testing the transplantation of islets that are encapsulated with a special coating designed to prevent rejection.
Shortage of Islets
A major obstacle to widespread use of islet transplantation is the shortage of islets. Although organs from about 7,000 deceased donors become available each year in the United States, fewer than half of the donated pancreases are suitable for whole organ pancreas transplantation or for harvesting of islets-enough for only a small percentage of those with type 1 diabetes.
However, researchers are pursuing various approaches to solve this problem, such as transplanting islets from a single donated pancreas, from a portion of the pancreas of a living donor, or from pigs. Researchers have transplanted pig islets into other animals, including monkeys, by encapsulating the islets or by using drugs to prevent rejection. Another approach is creating islets from other types of cells, such as stem cells. New technologies could then be employed to grow islets in the laboratory.